If you are woman in her 30s or 40s, you’re probably not thinking of menopause. And if you’re not thinking of menopause, perimenopause and osteoporosis or bone loss is something that is probably not on your radar.
But since 5-10% of women enter menopause before age 45, and because the symptoms, including bone loss, may begin up to 10 years before that, it’s something you should be thinking about.
Why? Because if you’re a healthy 50-year-old woman, your chances of dying of a broken hip are the same as your chances of dying of breast cancer.
The risk of osteoporosis goes up as you enter perimenopause and menopause nears, because estrogen levels are dropping. And estrogen is a key hormone that in addition to its many other functions, is responsible for repairing bones and keeping them strong.
Once your bones weaken, they can break more easily. Even everyday activities like walking, exercising or the occasional fall may be the thing that causes a break.
The good news is, there’s a lot you can do to treat and even prevent bone loss, no matter what your age is. Figuring out you have bone loss is key and preventing more is essential.
A Silent Epidemic
Here’s the problem…Most women who have osteoporosis don’t know it because until a bone breaks, because they don’t have any symptoms. And the risks of osteoporosis are not only breaking a bone; you might not be as independent after you break that bone due to less mobility.
Bones that can be broken include the spine, hip, wrists, ankles or other bones of the arms and legs. One of my patients broke her ankle walking out of the shopping mall when she didn’t notice the curb because of all the bags she was carrying.
And when bone fractures heal, they may be more painful over time and make it harder for you to be active.
Who’s at Risk?
Below is a list of risk factors for premenopause osteoporosis:
- A family history of osteoporosis
- A personal history of a bone fracture
- A long-time smoker
- Thin body, typically ≤ 125 pounds
- A history of anorexia or bulimia
- A history of kidney disease, celiac disease, thyroid disease
- Irregular periods for more than 12 months
- Too little or too much exercise
- Too little calcium or vitamin D
- Certain medications such as steroids, antiseizure meds, some chemotherapy drugs, and long-term use of the blood thinner heparin.
How To Lower Your Osteoporosis Risk
Some things are beyond your control. But not smoking, getting enough calcium and vitamin D, and getting the right amount of exercise are things that you can do to help lower your risk. Other bone health measures you can take include:
- Limit excessive alcohol
- Eat foods rich in calcium and vitamin D, such as milk, cheese and other dairy foods, green leafy vegetables, such as broccoli, cabbage and okra, but not spinach, soy, nuts and prunes all support bone health.Minerals that support bone health include boron, copper, and magnesium. Fish where you eat the bones, such as sardines are also good foods to support bones.
- If you aren’t getting enough calcium and vitamin D in your diet, consider nutritional supplements such as a multivitamin, calcium and vitamin D.
- Regular exercise, especially weight-bearing exercises like dancing, jogging, walking and tennis, and weight training.
- If you are found to have bone thinning, talk to your doctor about medications to strengthen your bones or at least prevent further bone loss.
Screening for Premenopausal Osteoporosis
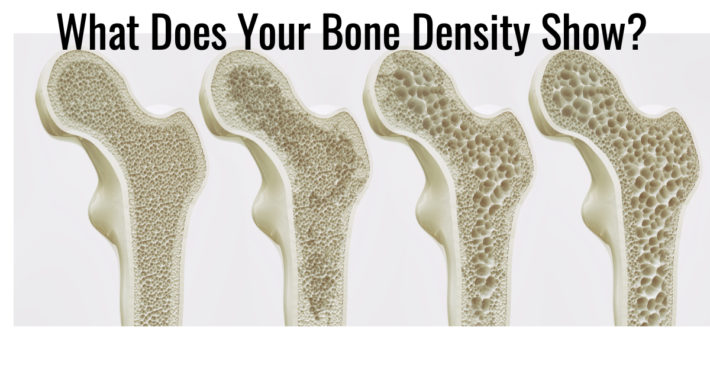
If you are at risk for a bone fracture or osteoporosis, talk to your doctor about getting a bone density. If you’ve had a broken bone in the past or a strong family history of osteoporosis, ask to get one at age 40. Even if you haven’t had a prior bone fracture, you should discuss getting a bone density at whatever age you enter menopause, especially if you go into early menopause or premature menopause (before age 40), and repeat in one to two years. It takes two dots to make a line to see if your bones are thinning or not.
How Is Premenopausal Osteoporosis Treated?
There are many treatments for osteoporosis. If you find you are losing bone and you are within three years of entering menopause, estrogen can actually help you get the lost calcium back into your bones. If you have been in menopause for seven years or more, estrogen won’t replace lost bone, but it will stop you from losing more. You can discover this and many more treatments in The Estrogen Fix.
There are also other treatment options for osteoporosis that may slow or even reverse bone loss.
Examples of those drugs include a bisphosphonate, such as risedronic acid (Actonel), alendronate (Binosto), alendronic acid (Fosamax), or ibandronic acid (Boniva). These as well as some other medications have been shown to help stop osteoporosis.
The most important thing is to realize you are at risk, and that bone loss is treatable and sometimes even preventable. Are you at risk? What are you doing to stop it? Leave your comments below.