Most women worry about breast cancer. Many don’t realize that they are ten times more likely to die of heart disease than breast cancer. I talk about this in great detail in my best selling book The Estrogen Fix. Here is some of what I talk about in the book.
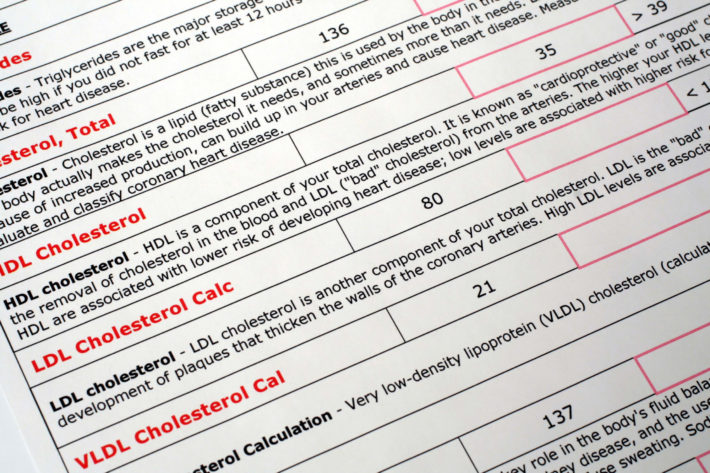
Lipids and Cholesterol and Your Heart
Lipids are fat-like substances in the blood and body tissues. Cholesterol is the main lipid, and it’s made up of different parts, such as HDL, LDL, and triglycerides, that I’ll talk about more shortly. Most people worry about their cholesterol levels. Nearly 100 million people take a cholesterol-lowering drug, and since the criteria for taking them were changed in November 2013, that number is rapidly increasing. Suffice it to say, with so many people taking these medications, you probably know that controlling cholesterol levels is important and that an increase of cholesterol is associated with heart disease. You might think that in general, cholesterol is bad.
Cholesterol, like most things, is not inherently entirely good or bad. Our bodies need cholesterol to insulate nerve cells in the brain and to create structure for the walls of cells. Cholesterol is also a basic molecule in the production of many of the body’s hormones. Seventy-five percent of cholesterol is made either by the liver or cells elsewhere in the body. The other 25 percent comes from food.
Like butter or vegetable shortening, cholesterol is a fat, and it doesn’t dissolve in the blood. To be transported throughout the body–fat and water don’t mix, and your body is mostly water–cholesterol attaches to proteins, and it’s the proteins that circulate in the blood vessels. Since this molecule is a combination of a protein and fat or lipid, it is called a lipoprotein. One type is HDL, or high-density lipoprotein. HDL is sometimes called good cholesterol because it is believed to mop up LDL from the blood vessel walls and remove it from the body. LDL, or low-density lipoprotein, is called lousy or bad cholesterol because it can build up in the walls of arteries and cause plaque that can narrow blood vessels and reduce bloodflow.
The plaque forms because LDL at higher levels can be absorbed into the artery walls and attract white blood cells (WBCs). The WBCs act like Pac-Men and eat the fatty particles to try and heal the blood vessel, but it doesn’t work well. Instead, inflammation and fatty deposits called plaque form and cause the blood vessels to stiffen and narrow. That, in turn, reduces bloodflow, increases blood pressure, and causes the heart to pump harder to push blood through the narrower, harder arteries. Eventually that can lead to chest pain, stroke, heart attack, and many other symptoms, depending on where the plaque forms. If you add extra body weight to lots of plaque, the pump you call your heart then has to pump blood through a narrower set of pipes to more pounds. That’s a lot of extra work for your pump.
Arteries, with progressively increasing amounts of plaque.
It’s also important to point out that different forms of LDL and HDL differ in how harmful or how protective they are. According to Dr. Steven Masley in his book The 30-Day Heart Tune-Up, LDL cholesterol can be small and dense or big and fluffy. The fluffy variety is packed with nutrients and carries fat-soluble vitamins and antioxidants to your cells. It’s the smaller LDL particles that are the problem; they cause plaque to grow, and that is believed to be because of their smaller size, which makes it easier for them to penetrate the lining cells of arteries.
LDL can be influenced by behavior. The more you stay physically active; eat fruits, vegetables, and healthy fats like unsaturated fats and omega-3s; and avoid refined carbohydrates and saturated and trans fats, the less small LDL you’ll have. Although oral estrogen is consistently found to lower the total levels of cholesterol and total LDL levels, only some studies suggest estrogen also helps to lower small LDL particles, while others suggest that oral estrogen increases small LDL particles.17, 18 In contrast, transdermal estrogen has little effect on either total LDL or HDL levels but does slightly decrease total plasma triglyceride levels and produce larger LDL particles that are resistant to oxidation, which is a good thing.19
HDL also comes in two sizes: HDL2, which is big and able to remove LDL and other negatives from the arteries, and HDL3, which is smaller and not very effective at removing the bad stuff from your arteries. So size does matter. Estrogen may play a role in increasing the HDL2 subfractions.
While the typical blood tests for HDL and LDL are accurate 80 percent of the time, according to Dr. Masley, that means they aren’t precise at predicting heart disease 20 percent of the time. If you are at high risk of heart disease, ask your doctor to check an advanced lipid profile.
So what role does estrogen play in heart disease in addition to influencing cholesterol levels? The walls of blood vessels have estrogen receptors where estrogen can have a direct impact. A particularly large number of estrogen receptors are in the blood vessels of the heart, the aorta, and the saphenous vein, which is a large vein in the legs. When estrogen attaches to these receptors, it activates certain genetic activity that helps these blood vessels dilate and improves the flow of calcium ions, which enhances bloodflow and has other beneficial actions. In laboratory studies done with arteries taken from menopausal women not taking estrogen, the arteries were found to function poorly. When estrogen was added to the culture dishes, the function of the arteries improved. In a study involving estrogen given to women after menopause, the women’s blood vessels responded to estradiol with the most dilation and improved bloodflow if the women were within 5 years of menopause. All this information points to the role that estrogen has on bloodflow in women and highlights the importance of taking advantage of your estrogen window for overall optimum health benefits. The closer to the beginning of menopause you start taking estrogen, the greater estrogen’s potential benefit to your heart.